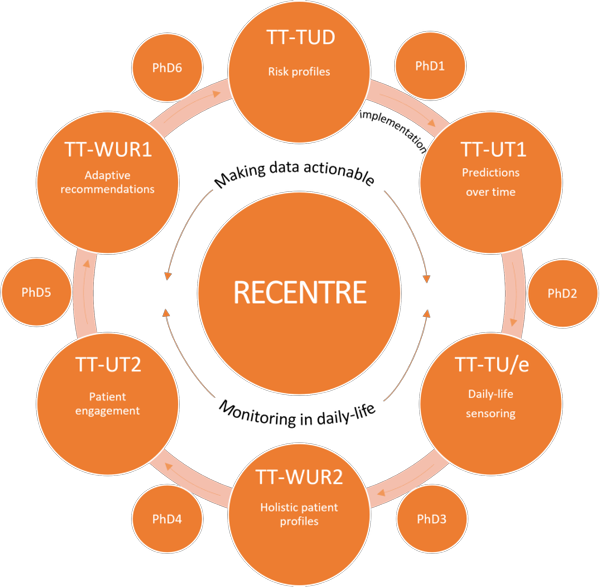
RECENTRE unites 4TU expertise in sensing, modelling, and implementation science to create cutting-edge, accessible eHealth solutions.
RECENTRE is a 4TU.Federation, a collaboration consisting of members of Wageningen University & Research, TU Delft, Technische Universiteit Eindhoven and University of Twente.